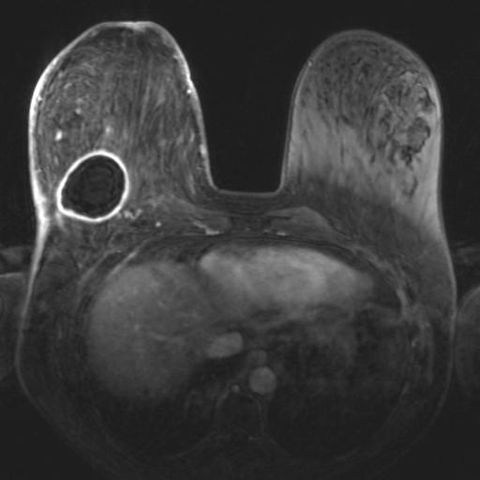
Breast MRI does not use X-rays and does not require breast compression.
Every day medicine fights a new battle. New studies lead to better results that translate into greater possibilities of prevention and cure. Magnetic resonance imaging (MRI) of the breast is a study that is being performed more and more because it has proven to be excellent in the battle against cancer. The number of clinical studies is increasing every year thanks to advances in technology that does not use X-rays or require compression to be applied to the breast. However, it is a more expensive and time-consuming study than mammography and sonomammography because it requires the injection of a liquid contrast medium for the evaluation of breast and underarm tissue. It is considered a complement – not a substitute – for mammography and sonomammography. It is true that it detects many cases of breast cancer that are not discernible by mammography or sonomammography, but the opposite is also true.
For a breast MRI to yield the desired results, it is imperative to establish that today only a minority of MRI machines in Puerto Rico have the capacity to study the breasts optimally. The equipment in which the breasts are studied must have a static magnetic field of 1.5 Tesla, being Tesla the unit of power of the magnetic field. Therefore, this requirement excludes all MRI machines with open architecture.
It is also a requirement that the breasts are studied with an ergonomically dedicated coil for both breasts. The patient lies face down, placing the breasts in a dependent manner in a kind of pit. Another requirement is a softeare program to analyze how the intravenous dye runs throughout the breast tissue. For the program to work, the MRI machine must have the ability to scan the entire breast tissue in less than a minute, repeating for several minutes. At present, the key to breast cancer detection by MRI is the level of detail that will help the trained breast MRI radiologist categorize the lesion(s). Not all MRI equipment of 1.5 Tesla or greater has the software or dedicated breast bovine.
The injection of intravenous gadolinium contrast is done by means of a mechanical injector in order to obtain an ideal amount of contrast in the bloodstream at the time of imaging. Manual injection is neither reliable nor recommended. All relevant precautions for patients who are at high risk for developing adverse reactions to contrast apply and should be taken into consideration by both your radiologist and referring MRI physician.
In addition to the technical factors described above required to perform a breast MRI optimally, the professional human factor is imperative. In order to responsibly interpret this study, it is vital that the radiologist master the basic physics and instrumentation aspects of the MRI modality in order to be aware of the myriad of artifacts that often arise that can result in false positive results (indicating cancer when there is none) and more importantly, false negative results (indicating no cancer when there is none).
Why Both Breasts Are Always Studied in the MRI Study
It is worth emphasizing that both breasts are always studied in the MRI study. Several publications have reported that MRI detects occult cancers (not palpable on physical examination) and cancers invisible on mammography and sonomammography in the breast opposite the breast in which a problem is suspected in 6% of cases. In the patient with breast cancer who has had a mastectomy, the follow-up MRI study is obtained to evaluate both the intact breast and the anterior chest wall of the mastectomy, whether or not breast reconstruction has been performed.
MRI-guided Breast Biopsies
The American College of Radiology (ACR) contemplates establishing as a requirement for the accreditation of facilities that practice breast MRI, that the imaging center provide the service of MRI-guided breast biopsy. This requirement further limits the places in Puerto Rico where a patient can currently undergo surgery when a suspicious lesion for cancer is detected that is only visible on an MRI. MRI-guided breast biopsy is reserved for those lesions that are completely invisible on mammography and sonomammography. Occasionally, a follow-up sonomammogram targeting the area of suspicion on MRI can reveal the elusive lesion and it can be biopsied without incurring the expense of MRI biopsy.
When to Have a Breast MRI
In women of reproductive age, breast MRI is performed on certain specific days of the menstrual cycle, otherwise, the results may show findings that simulate breast cancer when they are not. It is important to be patient to have the MRI done at the optimal time in order to obtain the most accurate and relevant information possible.
The breast MRI study has specific clinical applications including patients at high risk for breast cancer. These are those who have already been diagnosed with breast cancer; with breast cancer in close relatives (mother, sister and grandmother); and with positive genetics – BRCA-1 and BRCA-2 genes (breast cancer 1 and 2). When there are discrepant findings on other imaging modalities, MRI can help clarify them.
When the breasts are too dense on mammography, either because the patient is young and glandular tissue predominates over fatty tissue or because the patient is taking hormone replacement, glandular tissue can often hide cancer on mammography.
Because the principle on which MRI operates is independent of the dense breast, MRI is indicated for those patients who are clinically suspicious or at high risk for dense breasts on mammography. This same principle applies to patients who have had implants inserted to enlarge their breasts in whom mammography and sonomammography are limited for breast cancer detection. In fact, MRI is the study par excellence for evaluating the integrity of implants (whether they are ruptured or intact).
Other Applications When a Breast MRI is Performed Briefly Listed.
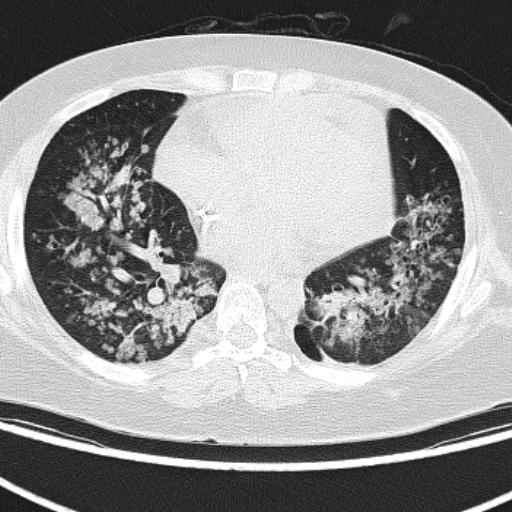
The study is performed before deciding how extensive surgery will be when a positive biopsy has already been obtained for cancer and it has been established that it has not progressed to other parts of the body. Often MRI reveals that the cancer involves other parts of the breast beyond what the mammogram suggests or what is clinically suspected including sometimes the surprise of discovering a second or third hidden cancer either in the same breast or in the opposite breast. In this way, MRI assists the surgeon in performing the most appropriate surgery feet you do not want to leave tumor unremoved nor do you want to remove too much non-tumor tissue when the patient wants to preserve her breast.
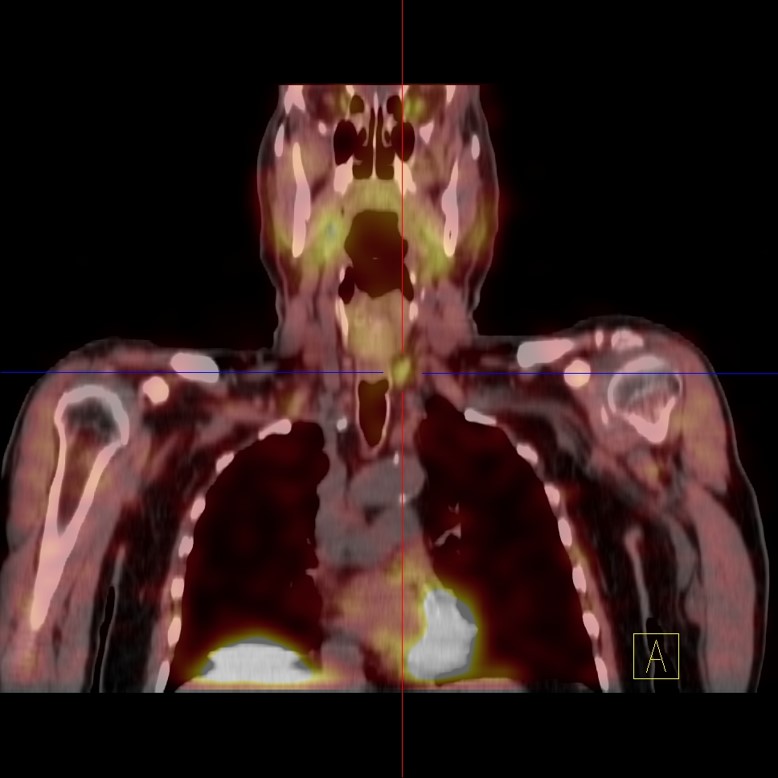
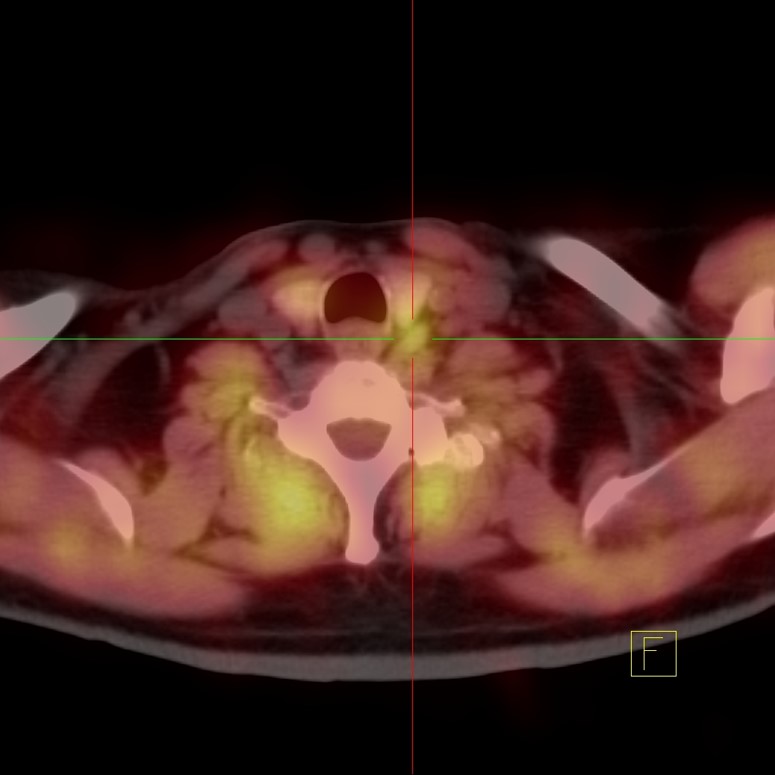
MRI is also indicated to assist the oncologist in establishing whether the cancer responds favorably to chemotherapy before surgery (neoadjuvant therapy). If the tumor shrinks significantly with therapy – if the tumor responds favorably – surgery is more likely to be curative.
Another indication for breast MRI is when a mammogram and sonomammogram reveal no cancer, but an axillary lymph node biopsy is positive for metastatic breast cancer. MRI is performed in search of the occult primary tumor responsible for metastasis to the axilla, in addition to several other indications that are being studied in these.
It is of utmost importance to note that at present no single imaging study is perfect for the detection of breast cancer or any other type of cancer, including breast MRI. The balance should be toward that combination of factors that maximizes the usefulness of this valuable contribution to improving the quality of life of the breast cancer patient.