Background
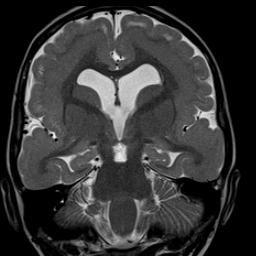
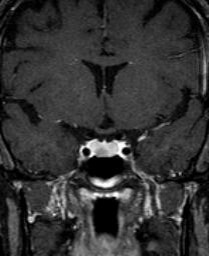
Magnetic Resonance Angiography (M.R.A.), also known as M.R.A. (Magnetic Resonance Angiography), is an application of magnetic resonance imaging (M.R.I. – Magnetic Resonance Imaging) that allows the non-invasive evaluation of arteries without using X-rays. Consistent with its rapid evolution, starting in the early 1990s, M.R.I. can be completed in seconds while its level of accuracy continues to improve. The venous angioresonance study, known as Magnetic Resonance Venography (M.R.V.), refers to the specific application to study the venous bloodstream. The addition of intravascular gadolinium eliminates the problem of overestimation of stenosis, reduces the number of false positive cases of total occlusion, and increases the accuracy of the calculation of the percentage of arterial diameter narrowing. This is due to the increase in information (signal) that paramagnetic contrast medium (gadolinium) provides, which in turn eliminates the problems of turbulent and tortuous flow previously presented by non-contrast MRI. Gadolinium also makes it possible to obtain branch detail of several major arteries as never before and reduces the possibility of patient motion artifact by lowering the study time from 8 minutes to less than 30 seconds.
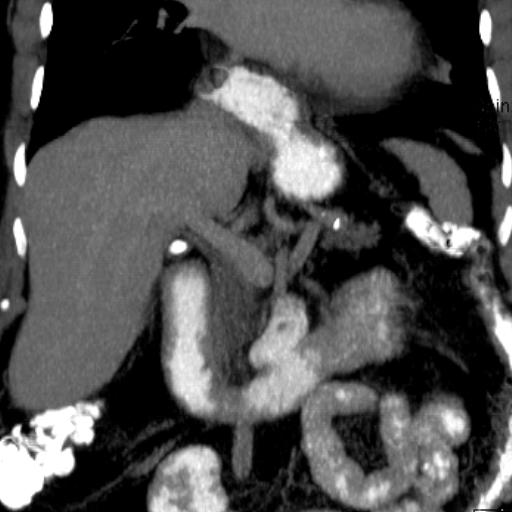
Computerized Tomography Angiography (C.T.A.) is an application of computerized tomography (C.T. Computerized Tomography) that allows the non-invasive evaluation of arteries using X-rays. While M.R.A. initially gained the lead, C.T.’s spiral miltidetector technology has advanced dramatically in recent years, matching and for some arterial beds surpassing M.R.A.
Replacement of D.S.A. by M.R.A. and C.T.A. and Role of Sonography
M.R.A. and C.T.A. studies have virtually replaced digital subtraction arteriography (D.S.A. – Digital Subtraction Angiography), also known as catheterization, in most cases for diagnostic purposes. The exception is the study of the coronary arteries. It is necessary that the patient cooperates and does not move during the precise moment of the study, otherwise it may be ruined, having to be repeated on another day. When there is doubt in the M.R.A. or C.T.A. study, the D.S.A. is recommended.
The D.S.A. test is invasive since it requires arterial puncture, catheterization, application of considerable doses of radiation, injection of iodine-based contrast and recovery time after manual or mechanical compression of the arterial puncture site. Other risks of D.S.A. are puncture site hematoma, embolization (blue toe syndrome and stroke), arterial dissection, pseudoaneurysm formation and arteriovenous fistula formation. Iodine-based intravenous contrast used in D.S.A. and C.T.A. is potentially nephrotoxic and has a higher incidence of serious adverse reactions, although the risk appears to be lower when administered by the arterial route. On the other hand, all M.R.A. studies use intravenous gadolinium-based contrast, except for the brain study which usually does not require it. As presented in previous editions of this journal, gadolinium is not nephrotoxic and has a lower incidence of serious adverse reactions compared to iodine-based contrast. However, if the patient is allergic to iodine-based contrast and has renal insufficiency, gadolinium administration should be done cautiously due to recent reports of an association with nephrogenic systemic fibrosis (JAMA, January 17, 2007 – Vol 297, No 3).
Of course, D.S.A. continues to be necessary for the performance of therapeutic procedures such as percutaneous transluminal angioplasty (P.T.C.A.), stenting, atherectomy and local administration of drugs such as T.P.A., urokinase and streptokinase, as well as chemotherapeutic agents.
Color Doppler (duplex) sonography represents the radiological modality most frequently used initially to study peripheral arteries due to its availability, lack of radiation use and lower cost. Unfortunately, the results are highly variable because they depend on the operator’s experience, knowledge of optimization of technical parameters and the quality of the equipment. Sonography has advanced significantly with the addition of spectral analysis with Doppler, the ability to encode directional information by means of color Doppler achievement and later with other techniques that include harmonic frequencies and power Dopper. Visualization of soft plaque is excellent on the new sonography units. When cholesterol plaque calcifies (hard plaque), the sonography artifact “shadowing” limits visualization of the arterial wall. When color is applied, the arterial lumen can be visualized more accurately.
Both C.T.A. and M.R.A. outperform sonography with or without color Doppler for several reasons. First, M.R.A. can perform a direct measurement of the vessel lumen, which is necessary to establish or rule out surgical criteria in the case of internal carotid narrowing, according to public studies. The surgical criteria established for the patient to benefit in the long term, reducing the incidence of stroke, has been described as narrowing of 60% or greater of the diameter of the artery in the European study; and 70% or greater of the diameter of the artery per study in the United States, using D.S.A. as the modality par excellence. Sonography establishes approximations of internal carotid artery narrowing in the necks offered in terms of ranges, e.g., 50-69%; 70-89%; etc. An estimated and indirect measure based on relative increases in blood velocity after the area of stenosis. The range of narrowing generated by sonography is too wide, as it includes the percentage of narrowing below the surgical criteria and above the surgical criteria (50-69%). The information on narrowing ranges was developed before the research on the established surgical criteria for internal carotid artery endarterectomy was published.
The sternum, ribs and lungs do not allow a reliable acoustic window to be obtained to probe the origin and course of the brachiocephalic, proximal left common carotid, proximal right common carotid, and proximal left subclavian arteries at the level of the aortic callus, so sonography cannot study these vertebral arteries is not evaluable by sonography. The vertebral arteries in the neck can be probed with high variability by sonography. Arteries in the pelvis, and sometimes in the abdomen, are not sondable because intestinal gas does not allow sound waves to penetrate the area of interest.
Establishing whether there is thermodynamically significant narrowing proximal to the cervical internal carotid (origin of the common carotid in the aortic callus) is highly relevant during surgical planning. It would not be useful to perform endarterectomy for a stenosis in the neck when one or more proximal stenoses coexist. At present, sonography cannot document proximal stenosis near the origin of the main arteries supplying the neck, face and brain in aortic callus.
Importance of the Type of Equipment in M.R.A. and C.T.A.
M.R.A. and C.T.A. studies should be performed with powerful magnetic field M.R.I. equipment measured in Tesla units. Open M.R.I. equipment at present, although it has shown substantial progress in recent years, is still not recommended for M.R.A. studies because it is much slower and its magnetic field is weak. M.R.A. acquisitions in an open machine take too much time, so they are more sensitive to the patient moving and ruining the study. The limitations of an open MRI increase the possibility that the angiographic image suggests that there is a narrowing or occlusion when in fact there is not, or that the presence of an aneurysm is falsely established – false positives, among other problems. Open equipment also does not obtain the resolution of “closed” or conventional equipment for M.R.A. studies.
To obtain the results published in the literature, A.R.M. should be performed in 1.5 Tesla equipment. Literature studies of A.R.M. on 3.0 Tesla equipment will begin to be published once the coil technology is revised to handle the data obtained with these new scanners.
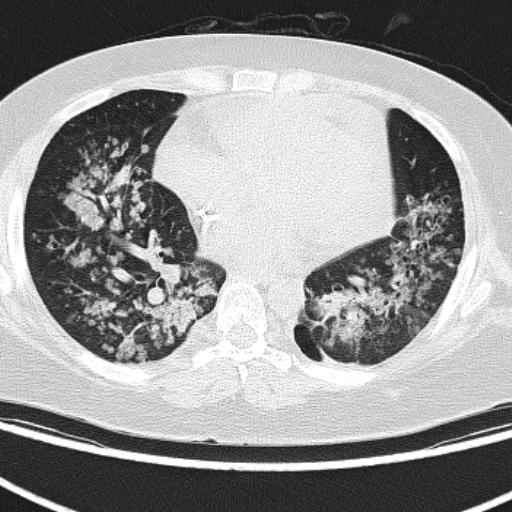
Similarly, to obtain the results published in the literature, C.T.A. should be performed on multidetector coils with the highest number of coils available. To date, 16-row X-ray detectors have provided the most reliable images for C.T.A. studies, except for coronary arteries for which a 64-row C.T. scanner is the new standard. At the time of this writing, C.T. technology continues to advance rapidly so that 128- and 256-detector-row equipment is being designed.
A German imaging equipment company launched a new concept two years ago to further improve coronary C.T.A., in which two X-ray tubes used simultaneously in the same scanner reduce the time it takes to obtain coronary artery information by eliminating in most cases the need to use beta blockers to reduce the pulse to 60 or less. The double X-ray tube CT also reduces radiation exposure to the patient by about 50%, which is considerable in these studies. At present, using 64 or more rows of CT equipment has no clinically significant benefit over 16 rows for C.T.A. or regular C.T. studies of other parts of the body. No double X-ray tube CT has yet been installed in Puerto Rico at the time of publication of this journal due to its prohibitive cost.
Studiable Anatomy and C.T.A. versus M.R.A.
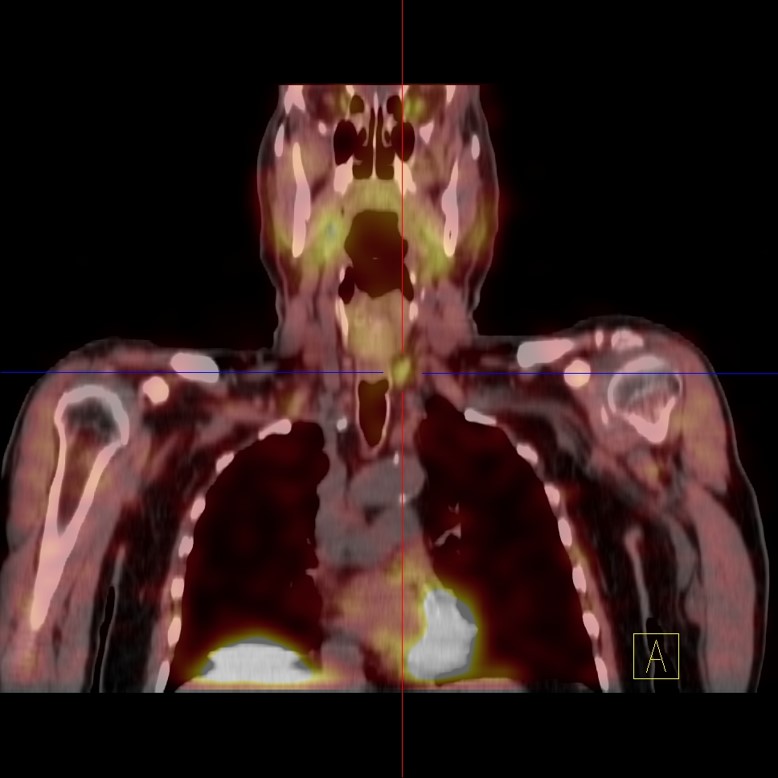
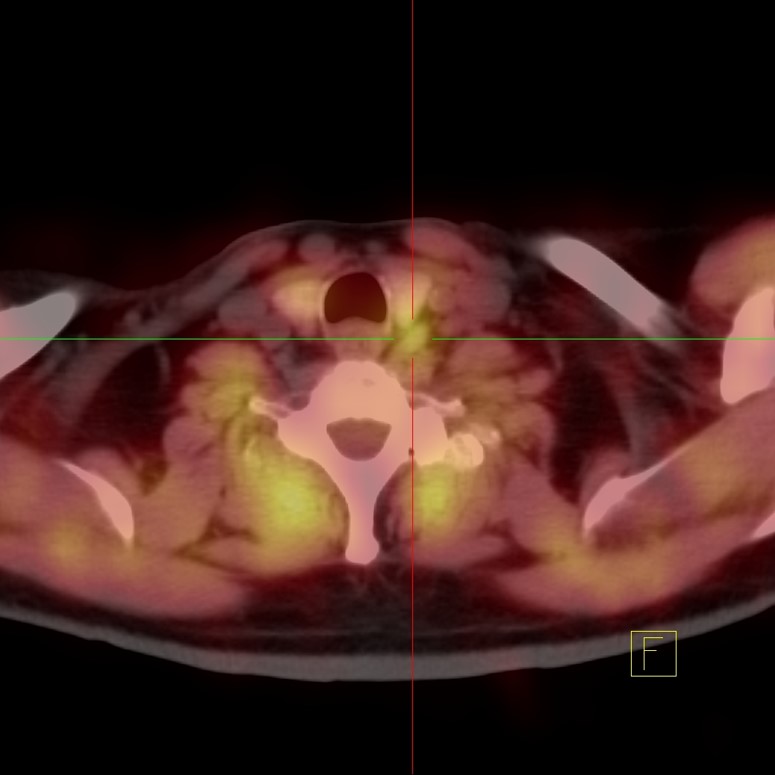
The anatomical regions in which M.R.A. and C.T.A. studies are routinely and robustly performed, when obtained on the advanced equipment described above, are: brain, neck, chest, abdomen and legs. Both M.R.A. and C.T.A. are less expensive than D.S.A. C.T.A. is superior to M.R.A. for the demonstration of hard (calcified) plaques. Like the M.R.I., the M.R.A. is not sensitive for the detection of calcifications. The C.T.A. uses radiation, but the M.R.A. does not. C.T.A. is less expensive than M.R.A. but uses potentially nephrotoxic contrast, while M.R.A. uses gadolinium which is not. It should be emphasized that with the exception of cerebral M.R.A., all M.R.A. studies should be performed with intravenous gadolinium contrast using an automatic injector.
M.R.A. vs. Coronary A.T.C.
For coronary arteries, C.T.A. in 64 detector rows or in double X-ray tube equipment represents the best alternative at the present time. Coronary C.T.A. is currently excellent as a screenin because it has an excellent negative predictive value so that when the study is negative, the patient avoids catheterization. Unfortunately, at present, when arteriosclerotic disease is detected, the stenosis calculation obtained by coronary C.T.A. is not sufficiently reliable to replace the stenosis estimate obtained by D.S.A. Coronary M.R.A. has progressed gradually, but multidetector spiral and double X-ray tube technology has made coronary C.T.A. surpass M.R.A. today.
Main Indications:
ARTERIAL (M.R.A. and C.T.A.).
- Detection and quantification of stenosis.
- Pulmonary embolism (C.T.A. exceeds in sensitivity and specificity to nuclear V/Q scan).
- Detection of vasculitis (granulomatous angiitis, fibromuscular dysplasia, Takayasu’s arthritis, etc).
- Congenital (cerebral) and arteriosclerotic aneurysm evaluation
- Arterial dissection
- Arterial supply and venous drainage of vascular malformations
- Arterial supply and venous drainage of tumors.
- Subclavian steal
- Anatomical variants (persistent connection between anterior and posterior cerebral circulation)
VENOUS (M.R.V.)
- Thrombosis and occlusion of cerebral dural sinuses with clinical picture of venous infarction.
- Narrowing vs. occlusion (renal carcinoma)
- Aneurysm (vein of Galen in brain)
- Anatomical variants
Comments
With the continuous technological evolution, M.R.A. and C.T.A. vascular studies have proven to be robust and reliable techniques, crucial tools for medicine in general for the benefit of patients, in particular for those with vascular disease who are typically hypertensive and/or diabetic. M.R.A. and C.T.A. performed on advanced equipment constitute a real alternative comparable to D.S.A. (except for coronary arteries as presented) and, although more expensive, superior to sonography. Since M.R.A. does not apply radiation or use nephrotoxic contrast, it represents an alternative for patients with renal problems.
Sonography with color Soppler and D.S.A. will not disappear. D.S.A. will continue to be necessary for therapeutic interventions, including angioplasty, stenting, embolization and local and remote infusion of thrombolytic and neuroprotective agents, whose applications continue to expand. Sonography is less expensive, but presents limitations particularly in the neck and pelvis.
About the author:
Dr. Fernando Zalduondo Dubner, Director San Patricio MEDFLIX, www.spmedflix.com, (787) 620-5757; (787) 766-1493.