Nuclear medicine has evolved in the last decade through the development of hybrid equipment that combines in the same box a nuclear camera with a radiology camera, either a CT scanner or an MRI scanner. Hybrid equipment combines physiological information from nuclear medicine with anatomical information from radiology. The result is a study that provides superior information that very often alters the diagnosis and treatment of the patient by avoiding surgery when it is unnecessary, by corroborating when surgery is necessary and by eliminating or reducing additional unnecessary studies. It also avoids the administration of ineffective chemotherapies by reducing their cost and complications and, when available, providing additional opportunities for palliation or cure when second-line or experimental therapies are available.
In the case of PET-CT, a PET (positron emmission tomography) camera is combined with a CT scanner.
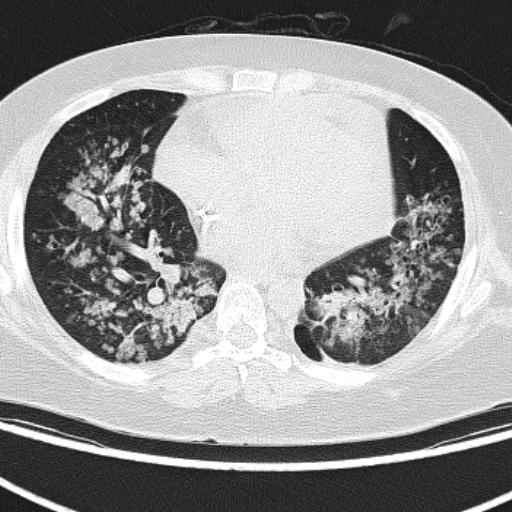
For years, gamma cameras have had the option of performing SPECT (single photon computed tomography) tomography slices to increase their sensitivity and sometimes their specificity. The inclusion of a CT scanner to SPECT gamma cameras has revolutionized the usefulness of several nuclear medicine studies, including bone scan, thyroid scan with iodine 131 and myocardial perfusion scan.
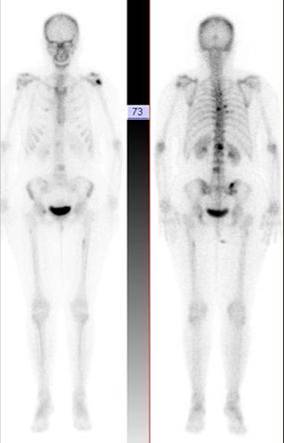
Image 1
Bone scan planar in breast cancer patient. Multiple dark spots on skeleton, suspected for metastasis
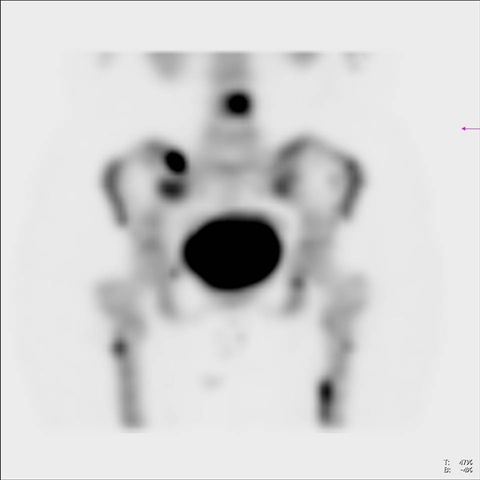
Image 2
Bone scan, pelvic SPECT, lower lumbar spine and upper thighs. SPECT detects additional lesions to those suggested by planar image (image 1)
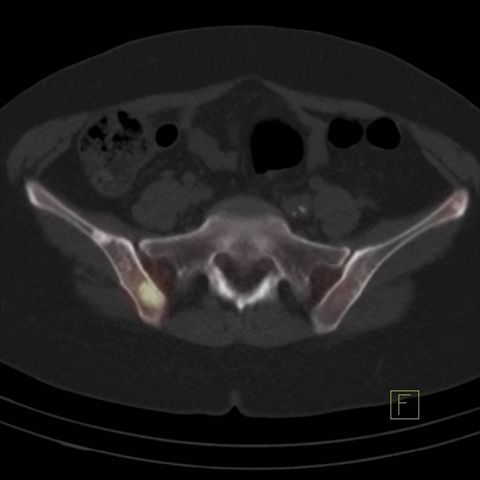
Image 3
Bone scan, fused image of SPECT and CT in pelvis Hot lesions are sclerotic and consistent with metastasis
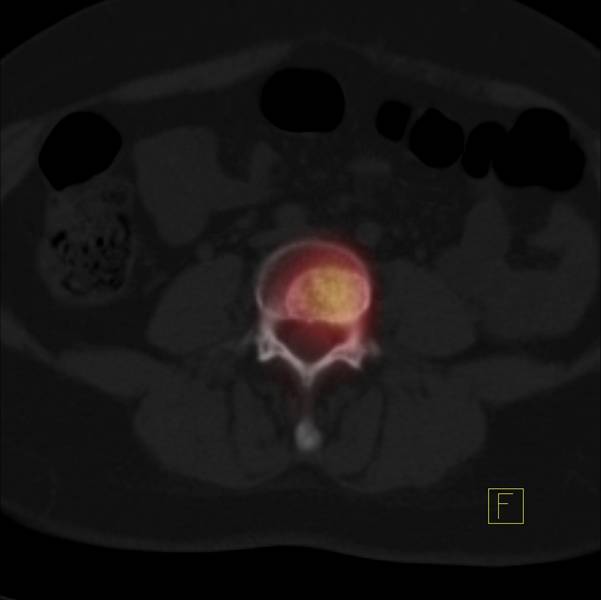
Image 4
Bone scan, fused SPECT and CT image in lower lumbar spine confirming spinal metastasis
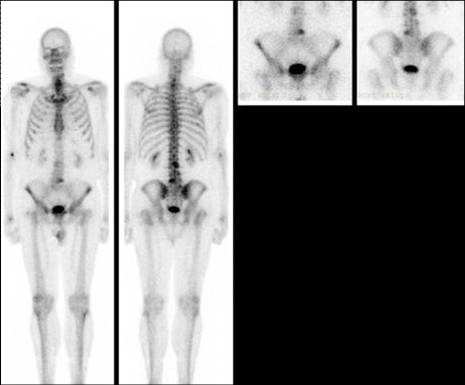
Image 5
Bone scan, planar images in a patient recently diagnosed with prostate cancer. Some lumbar spine lesions suspicious for metastasis

Image 6
Bone scan, lumbar spine SPECT visualizes better lumbar spine lesions, suspicious for metastasis

Image 7
Bone scan, SPECT and CT fused image of lumbar spine

Image 8
CT scan of the SPECT-CT shows that hot lesions on images 5, 6 and 7 are sclerotic but radiologically they are typical of chronic spondylotic disease and do not represent metastatic disease
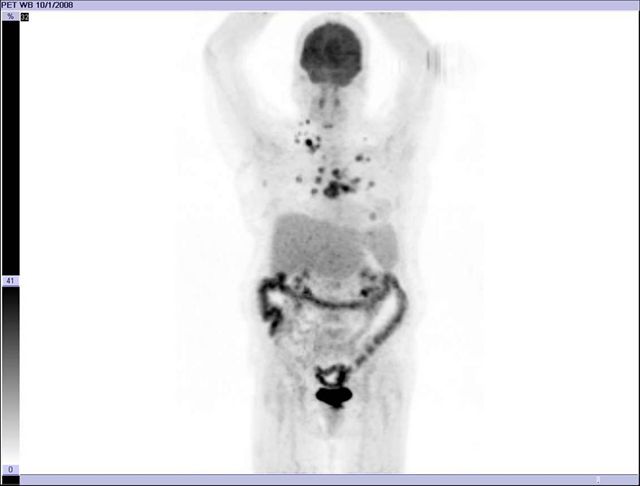
Image 9
FDG PET-CT, 3D image of normal PET. Physiological distribution of the tracer. Brain, liver, colon, kidneys and bladder

Image 10
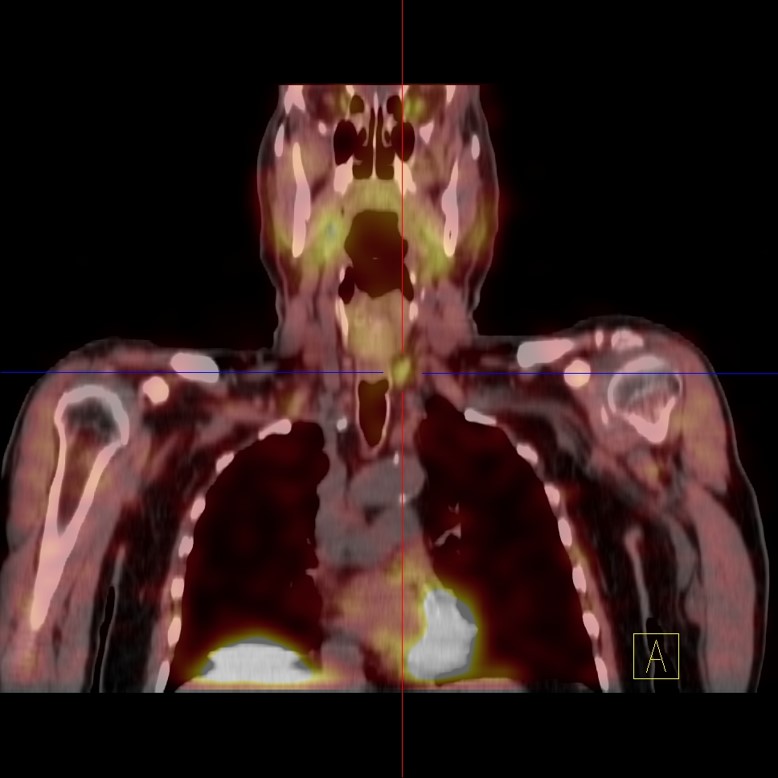
FDG PET-CT, breast cancer, base. Hypermetabolic hot spots consistent with metastasis
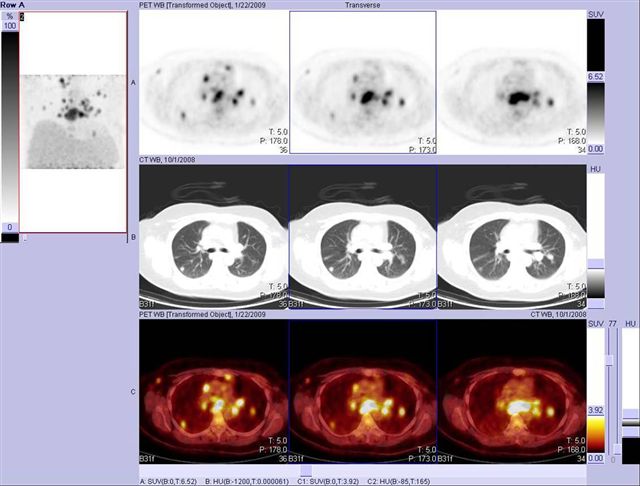
Image 11
FDG PET-CT, breast cancer, basal, lung (non-calcified nodes) and mediastinal lymph node metastases

Image 12
FDG PET-CT, same patient from images 10 and 11 obtained after few cycles of chemotherapy to evaluate metabolic response shows favorable response
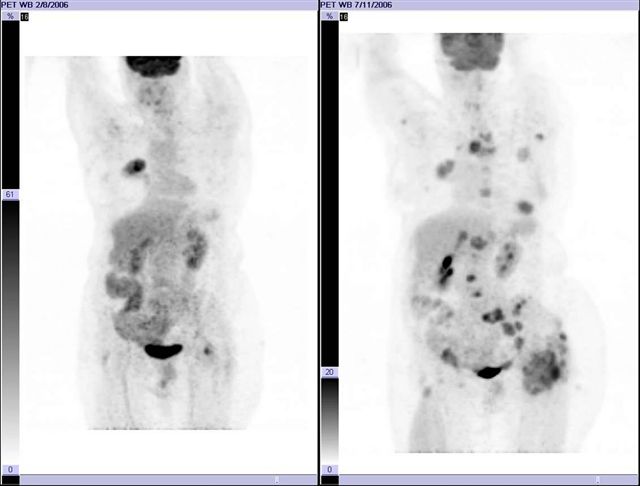
Image 13
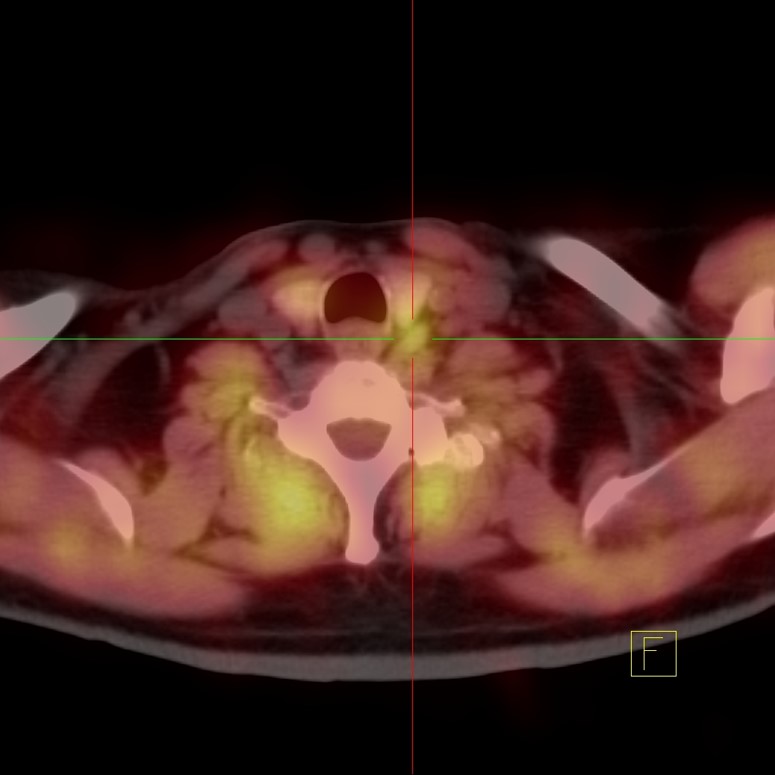
FDG PET-CT, 3D base and follow-up PET image after chemotherapy in patient with pulmonary adenocarcinoma The disease has progressed in 5 months. No follow-up study was obtained in a shorter period of time to establish whether the therapy was being effective or not
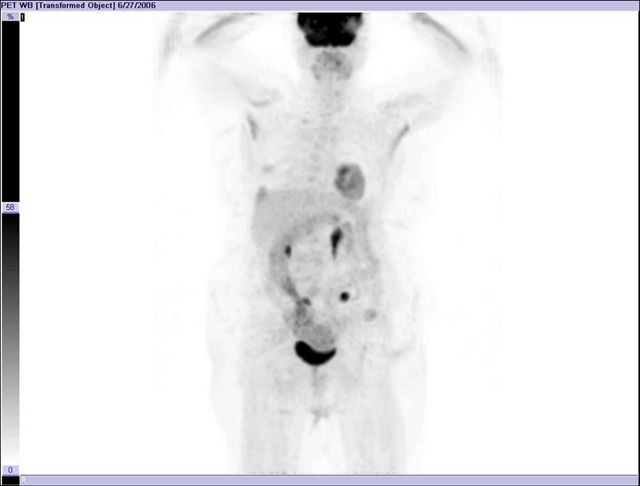
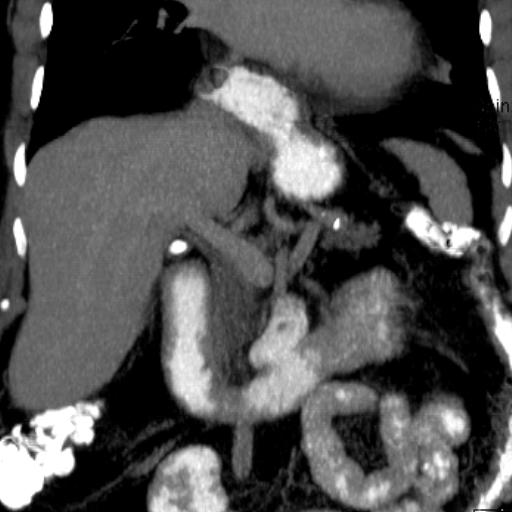
Image 14
FDG PET-CT, 3D PET image, colon cancer surgery patient presenting with elevated blood marker CEA series. CT scan negative. Suspicious spots in abdomen
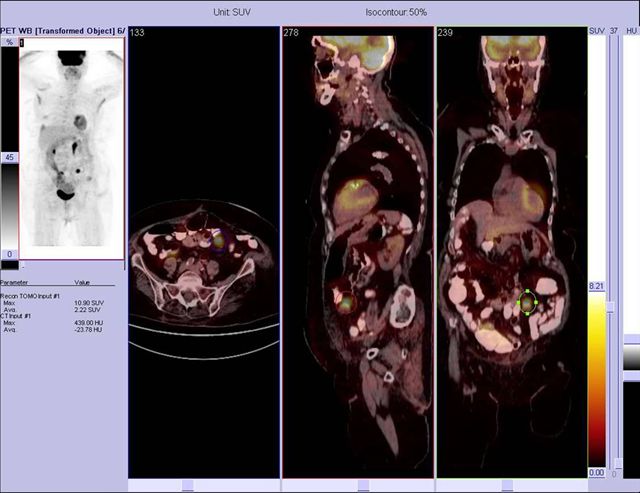
Image 15
FDG PET-CT, fused images show focus corresponding to a metastatic peritoneal implant correlating with recurrence and elevation of the CEA marker
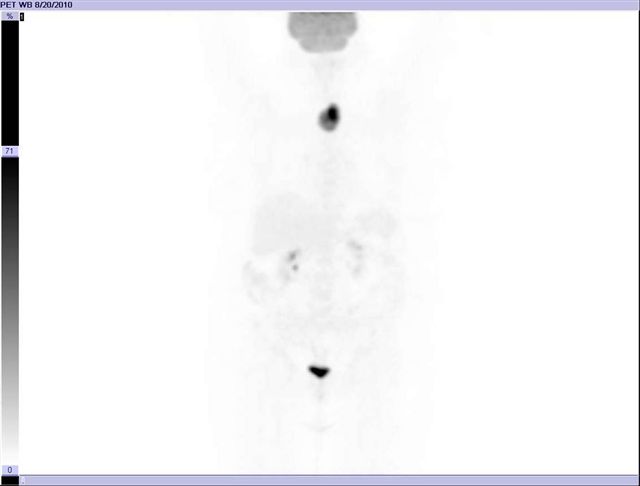
Image 16
FDG PET-CT, 3D image of the PET, shows abnormal focal activity in the lower neck, possibly in the thyroid gland. This finding is incidental because the patient presented as a follow up of a lymphoma
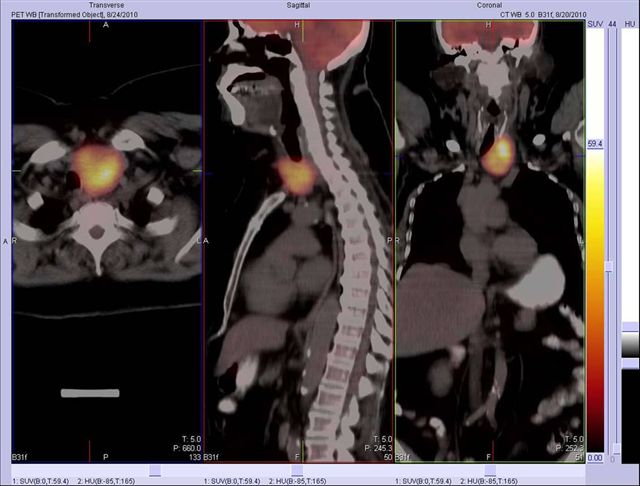
Image 17
FDG PET-CT, fused images confirm that there is a new hypermetabolic mass in the thyroid that proved to be a new primary cancer not clinically suspected. Incidental tumors are frequently detected in PET-CT studies
Image 18
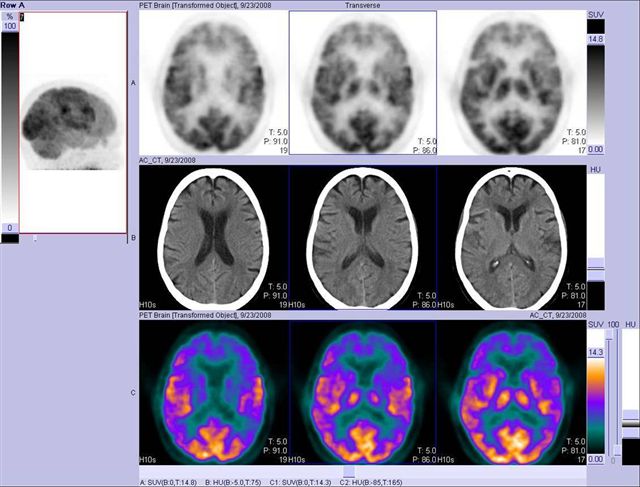
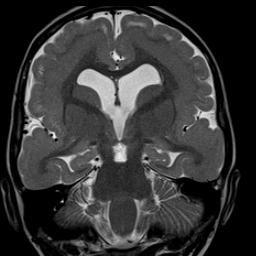
FDG PET brain, 3D image, shows normal tracer distribution. Basal ganglia accumulate FDG, normal
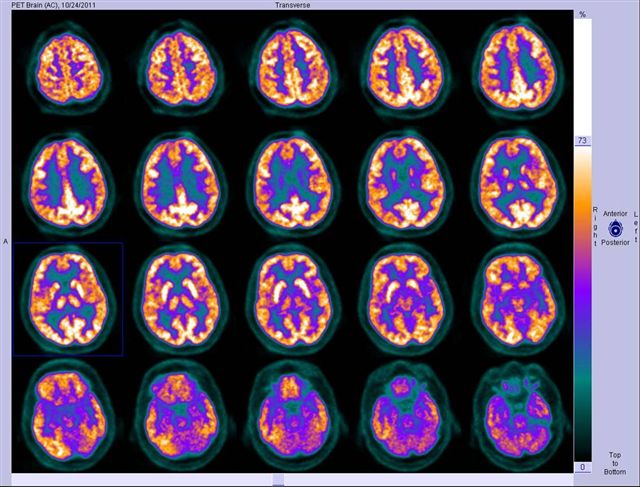
Image 19
FDG PET-CT brain. Color axial images show normal distribution in the cortex of all brain lobes
Image 20
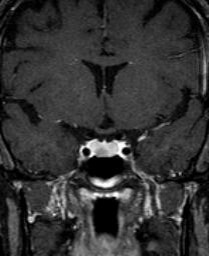
FDG PET-CT brain, 3D image, shows abnormal decreased cortical distribution in temporal lobes, back of frontal lobes and front of parietal lobes. Pre-central and post-central cortex (motor and sensory respectively) are not involved. Distribution is typical for Alzheimer's disease
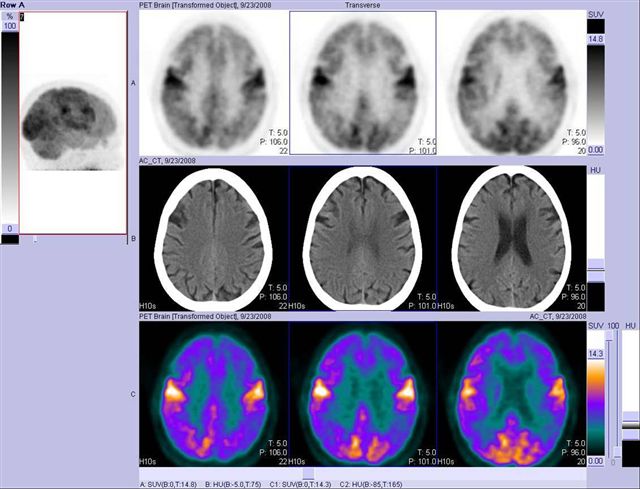
Image 21
FDG PET-CT brain. Three rows of tomographic images, from top to bottom, PET, CT and color PET, confirm in more quantifiable detail image findings 20. Distribution is typical for Alzheimer's disease