Neuroradiological anatomical studies include the brain, the spine, and the anatomy attended to by the otolaryngologist. For brain studies, for the vast majority of indications, MRI is the study of choice, although more expensive than CT. However, the CT scan, although using ionizing radiation, continues to be more available and the first line study particularly in emergency rooms and in the clinical setting of trauma, suspected subarachnoid and subdural hemorrhage and suspected recent cerebral infarction. When head trauma is suspected, negative calvarium radiographs do not rule out fracture, much less brain damage. To evaluate hyperacute cerebral infarction (images 3, 4 and 5), white matter disease (multiple sclerosis, vasculitis, among many others; images 6 and 7), cranial nerves (image 10), masses (images 13, 14 and 15), the pituitary gland (image 16), the pineal gland, among many other indications, MRI is the study par excellence, often requiring intravenous gadolinium contrast.
The definitive evaluation of the sinuses and the temporal/mastoid bones and bone labyrinth is performed with CT. MRI without and with intravenous gadolinium complements both studies, most frequently the temporal bones when seeking to distinguish recurrent cholesteatoma from scar tissue and for the evaluation of the membranous labyrinth and the nerves of the internal auditory canals. The evaluation of cerebral dysgenesis is performed with wide superiority with MRI over CT (image 12).
The evaluation of cerebral vascular malformations (image 9) is performed by MRI without and with gadolinium. The evaluation of cerebral aneurysms is performed by MRA or CTA. Please refer to the previous section that outlines these non-invasive modalities to study the blood vessels. The best evaluation of the venous dural sinuses in the brain is done by the combination of MRI without and with gadolinium and MRV (see image 1).
Evaluation for most neck and orbit indications is optimally performed with neck MRI and orbit MRI respectively, both without and with gadolinium. Some indications such as stone detection in the salivary glands and ducts are best performed with CT.
The spine is studied by segments to achieve sufficient detail so that for both CT and MRI, studies of the cervical, thoracic and lumbosacral spine represent separate anatomical regions. MRI, in addition to not using ionizing radiation, demonstrates the presence of herniated discs and various masses in a consistent and reliable manner. CT scans of these regions of the spine do not allow evaluation of discs in some segments and do not allow differentiation between recurrent herniated and scarred discs in the normal spine. MRI is superior during the evaluation of disc infection and adjacent vertebrae and for most cases of metastatic disease.
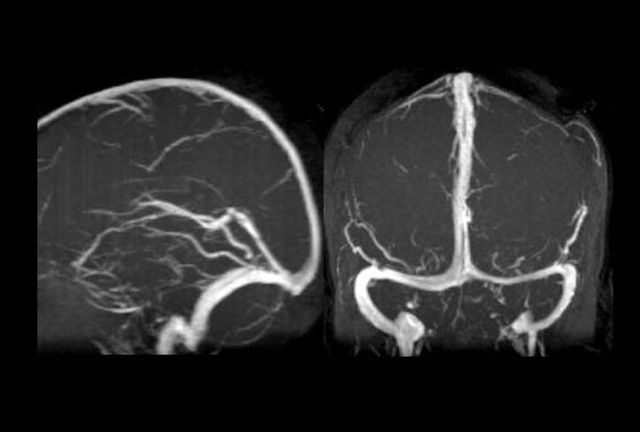
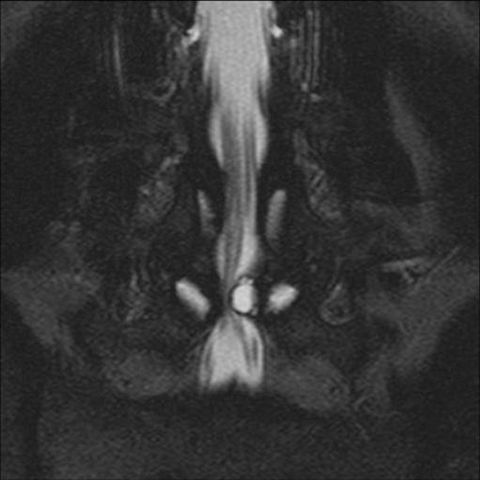
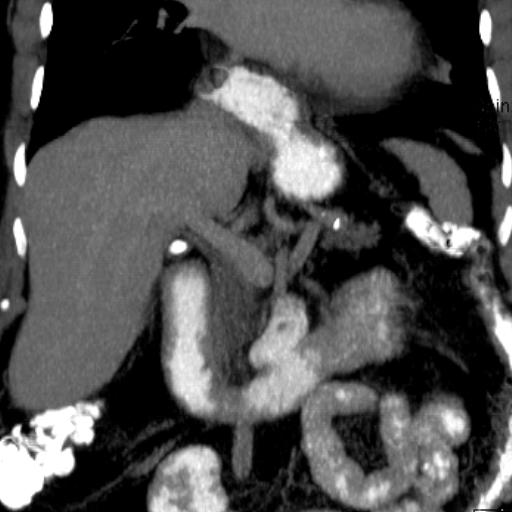
Image 1
Brain MRV. Sagittal/lateral and coronal/frontal views show normal flow. In coronal imaging, asymmetry in size of the transverse and sigmoid dural sinuses is normal, one side being dominant

Image 2
CT brain in patient presenting neurological deficits related to sudden vision loss. Negative study for infarction and hemorrhage
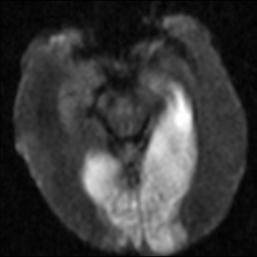
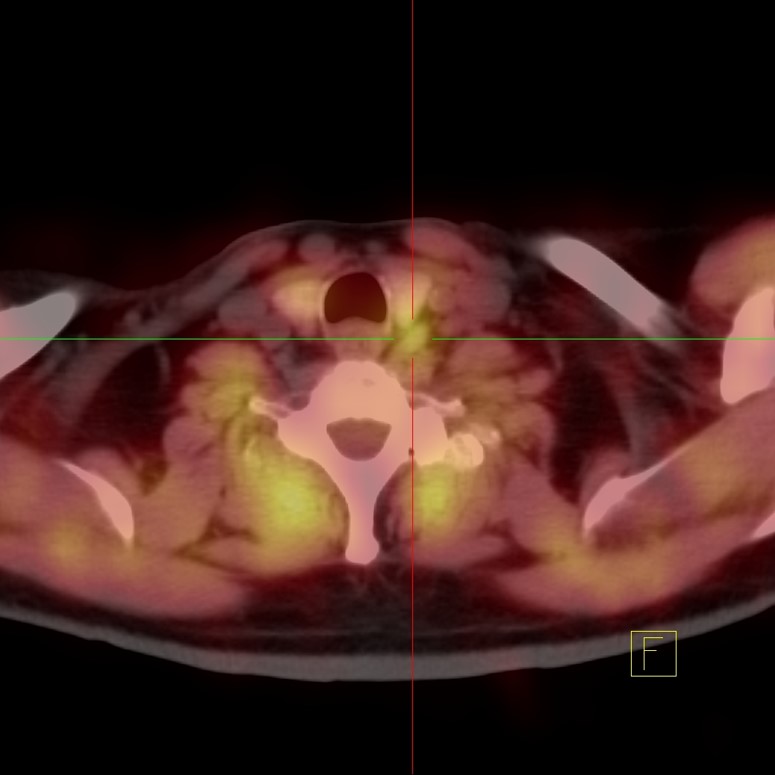
Image 3
Diffusion-weighted brain MRI (DWI) shows bright areas in right and left occipital lobes and left temporal lobe
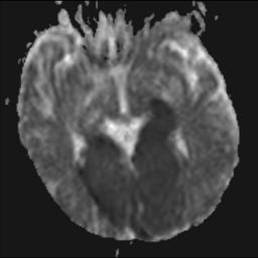
Image 4
Brain MRI, apparent diffusion coefficient image (ADC map) shows dark areas corresponding to the distribution of the abnormality in image 3, confirming very recent infarctions/strokes that explain neurological deficits. CT was negative at this early stage (image 2)
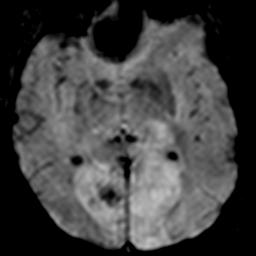
Image 5
Brain MRI, gradient echo image (GRE). This type of image is sensitive to the presence of bleeding by displaying it as black dots in this case
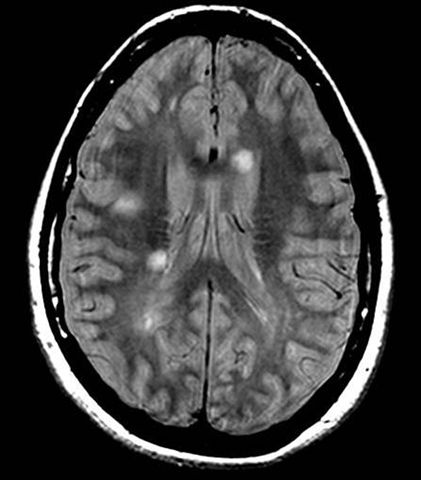
Image 6
Brain MRI. Patient with progressive numbness in various parts of the body. Multiple bright white matter lesions with peculiar orientation, typical for demyelinating disease such as but not limited to multiple sclerosis. Some conditions present similarly in MRI to multiple sclerosis, including Lyme disease
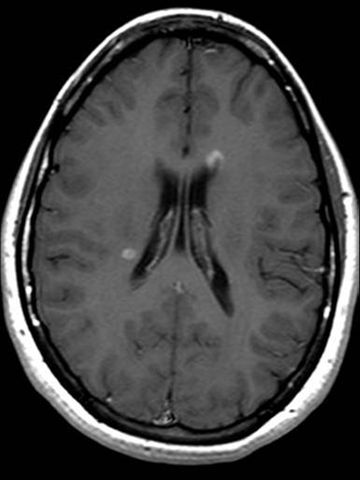
Image 7
Brain MRI with intravenous gadolinium from the same patient in image 5, shows that some of the lesions capture contrast, in this case representing active demyelinating plaques

Image 8
Brain CT of the same patient from images 6 and 7, negative. MRI is superior and preferred over CT for the evaluation of white matter disease, in this case having been proven as multiple sclerosis
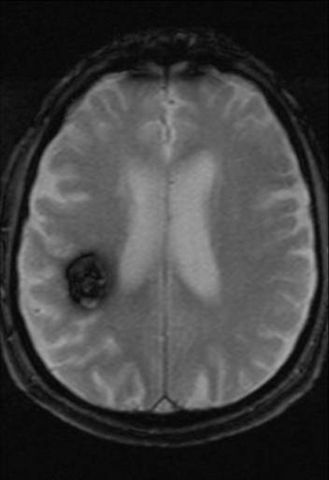
Image 9
Cerebral MRI, gradient echo image (GRE) shows black lesion in right frontal lobe with features typical for cavernous-type vascular malformation, also known as cavernoma. This type of image is sensitive to the presence of chronic bleeding by displaying it as a black area. The lesion must be followed up with MRI, not CT. CT scan in this patient was negative

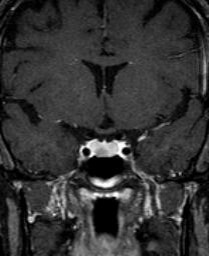
Image 10
Cerebral MRI with intravenous gadolinium in a patient with facial paralysis Coronal/frontal reconstruction dedicated to facial nerves shows that the right facial nerve captures gadolinium more avidly than the left, correlating with clinical presentation of Bell's palsy. The study ruled out that a facial nerve tumor or other condition was responsible for the clinical presentation
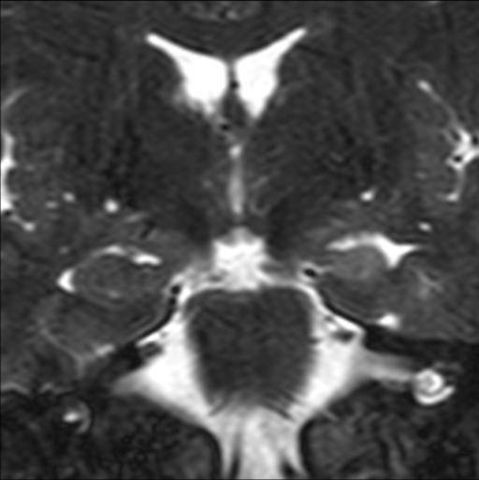
Image 11
Brain MRI, coronal/frontal oblique image dedicated to hippocampus in temporal lobes in young patient with partial complex epilepsy. Left hippocampus is atrophied and brighter than the right one. Diagnosis: mesial temporal sclerosis. Removal of the wrapped hippocampus eliminated epilepsy in this patient
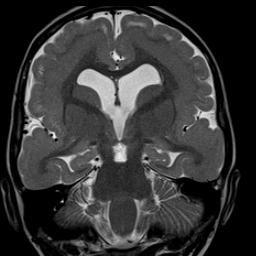
Image 12
High resolution coronal/frontal brain MRI. Small, cortex-identical signal node located in the occipital horn of the right lateral ventricle represents a migration disorder of gray material, in this case a subependymal heterotopia. Heterotopy refers to gray matter that did not migrate from its original position to the cerebral cortex. Detection of these findings requires high-resolution acquisition. These patients may present with developmental disorders and/or epilepsy, including
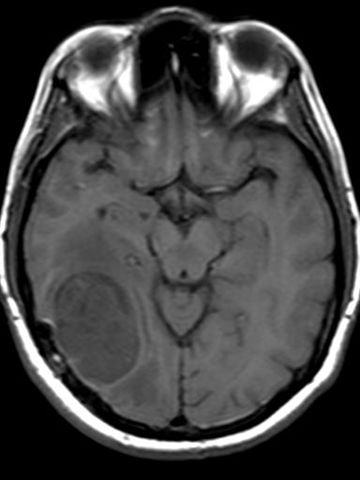
Image 13
Brain MRI shows a somewhat dark mass in the right hemisphere
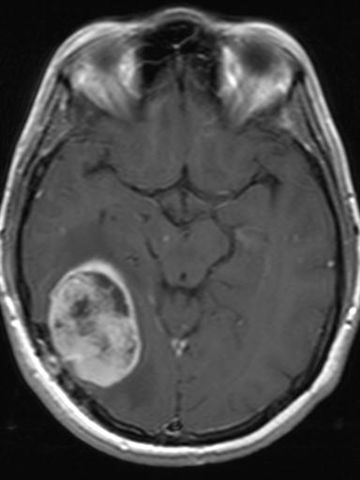
Image 14
Brain MRI of the same patient from image 13 after administration of intravenous contrast shows that the mass captures contrast in a heterogeneous way. This is an example of the more aggressive tumor that originates in the brain, glioblastoma multiforme
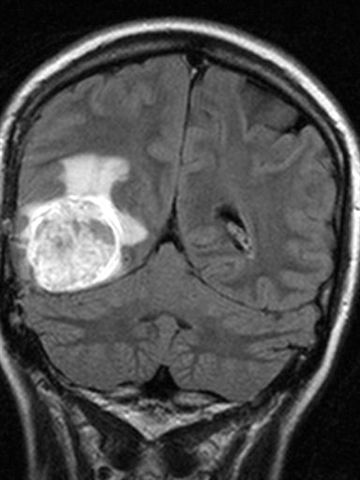
Image 15
Brain MRI of the same patient as image 13. This type of image demonstrates extensive vasogenic edema produced by the tumor. This type of tumor extends microscopically into the area of edema beyond what the gadolinium image suggests
Image 16
Brain MRI with gadolinium contrast dedicated to the pituitary gland demonstrates a lesion that captures less contrast than the rest of the anterior lobe, typical for a pituitary microadenoma. These lesions can be hormonally active and responsible for a variety of endocrine symptoms.

Image 17
MRI orbits without gadolinium show no abnormalities. Eyes and optic nerves show symmetry

Image 18
MRI orbits with gadolinium and fat suppression show that the left optic nerve picks up gadolinium diffusely without mass consistent with optic neuritis. Patient also had cerebral MRI demonstrating demyelinating lesions typical for multiple sclerosis. Many but not all patients with optic neuritis represent a manifestation of multiple sclerosis
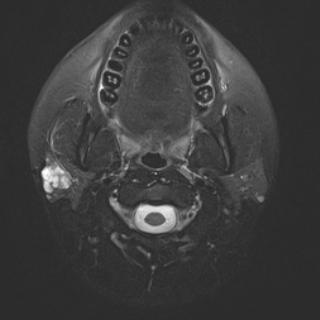
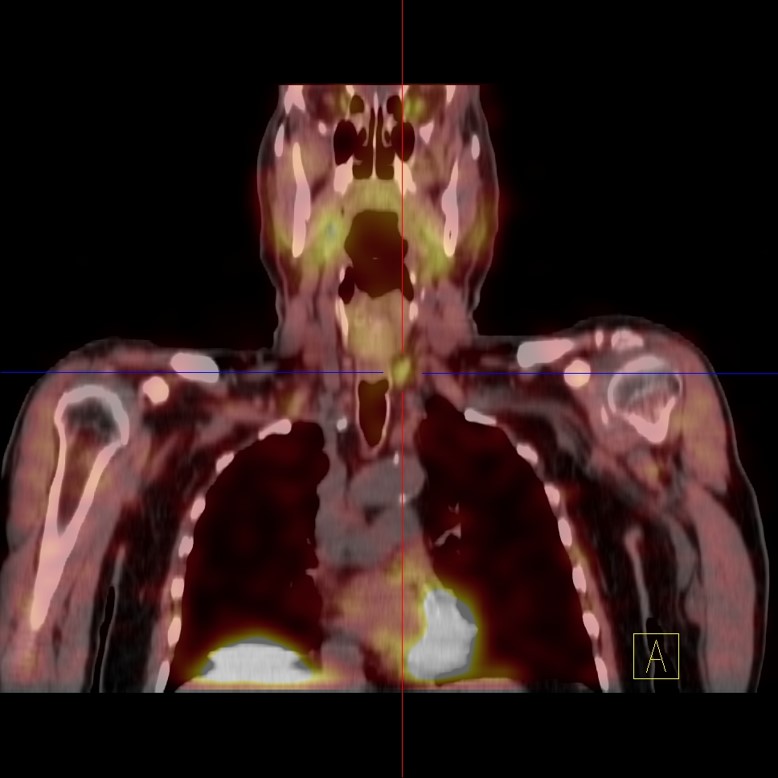
Image 19
Neck MRI. Bright lesion on right parotid gland
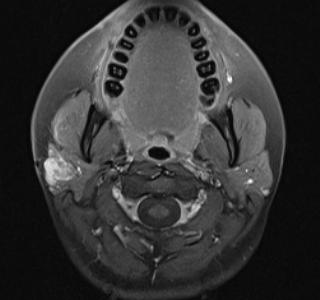
Image 20
Neck MRI with gadolinium. The same lesion in image 19 captures gadolinium excluding a single cyst and confirming the solid character that proved to represent a benign primary mixed-cell tumor originating in the parotid gland. MRI is superior to CT for most neck applications, particularly for the evaluation of non-stone pathology in the major salivary glands

Image 21
CT cervical spine by C6-C7 disc. Neither the disc nor the spinal cord are visualized due to the inherent artifact of the CT modality at this level due to the presence of shoulder bone
Image 22
MRI cervical spine by disc C6-C7 shows that there is no disc pathology at this level and that the spinal cord is normal in the same patient as image 16. There is no spinal stenosis
Image 23
MRI cervical spine shows herniated disc compressing the spinal cord and resulting in spinal stenosis
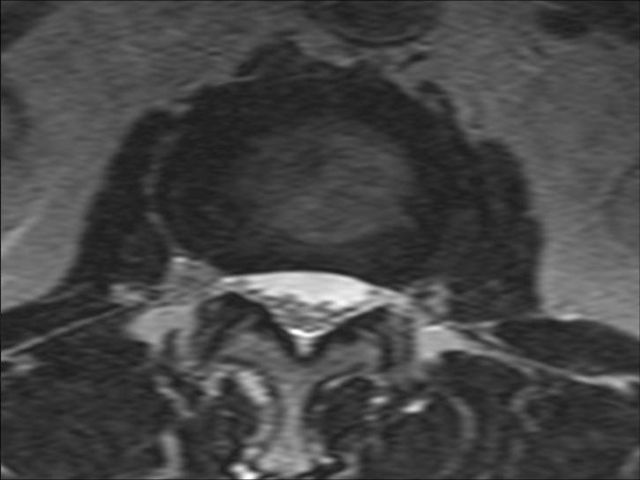
Image 24
MRI lumbar spine shows normal disc and normal ponytail. There is no spinal stenosis
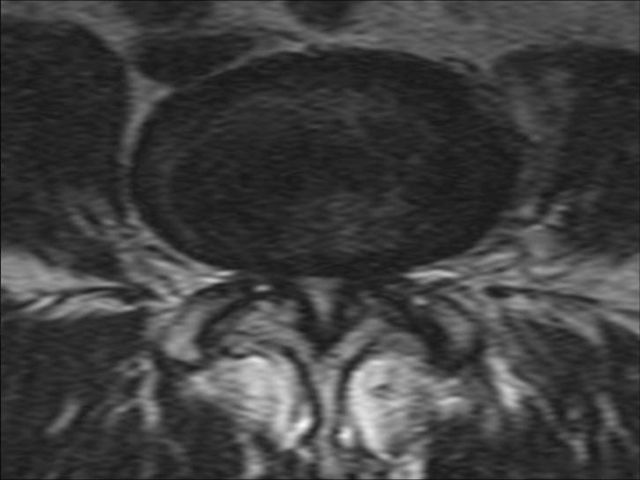
Image 25
MRI lumbar spine in another patient demonstrates arthritis in the facet joints (posterior elements) resulting in spinal stenosis of the central canal and both lateral recesses
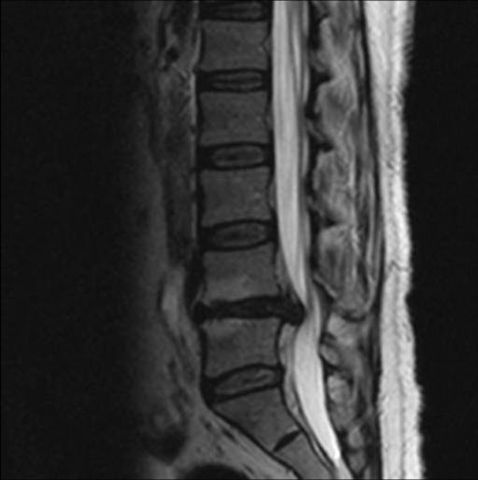
Image 26
Lumbar spine MRI demonstrates degenerative changes of the L4-L5 disc and a focal disc herniation. Spondylotic changes at L4 and L5 adjacent to the diseased disc are evident

Image 27
MRI columna lumbar del mismo paciente de la imagen 21 demuestra una herniación focal hacia el lado derecho del disco L4-L5
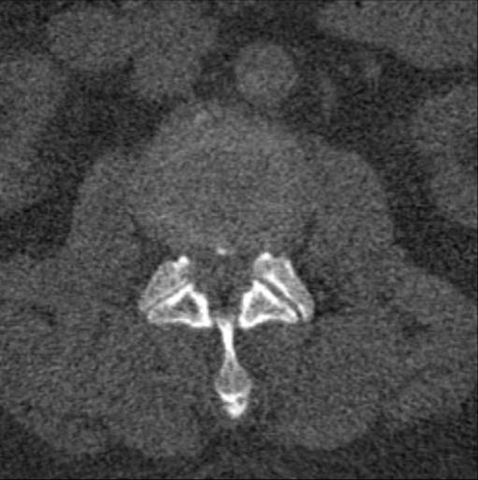
Image 28
CT scan of lumbar spine in thick patient suggests herniated disc but detail is not enough
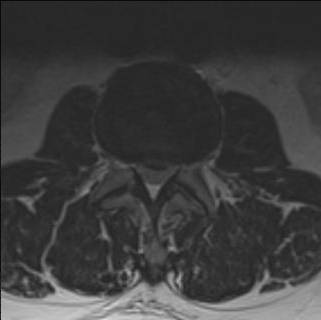
Image 29
MRI of lumbar spine in patient on image 28 demonstrates with certainty the presence of a herniated disc. MRI is superior to CT in demonstrating herniated discs, particularly at some levels (see CT image 21 which shows no area of interest)

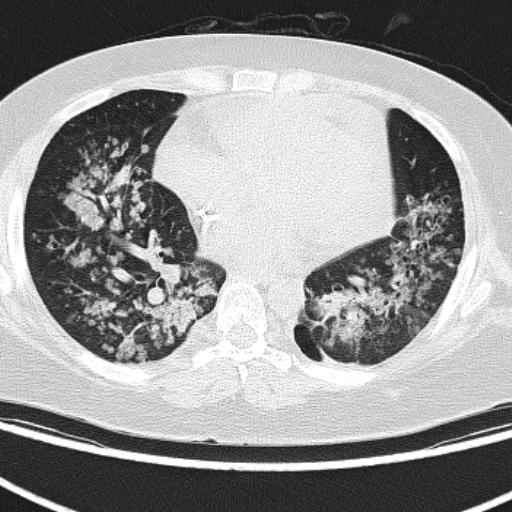
Image 30
MRI of the lumbar spine demonstrates degenerative disc disease and adjacent spondylotic disease in the bone marrow from three consecutive levels. Spondylotic changes in the bone marrow present a wide variety of appearances so it is imperative to know all their presentations to avoid misdiagnosis such as infection or metastatic disease
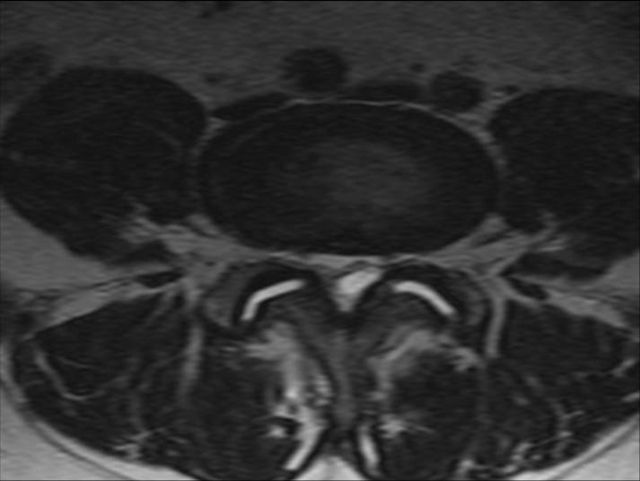
Image 31
MRI lumbar spine axial image demonstrates arthritis of both facet joints and a posterocentral cystic lesion adjacent to the facets compressing the tecal sac and its contents