According to the American Heart Association, cardiovascular disease has been the leading cause of death in the United States for over a century. Despite all the medical advances, statistics continue to be bleak with every 34 seconds a person dies in the US of a cardiovascular condition being the number one cause of morbidity and mortality. This points to the urgent need for new methods of diagnosis, prevention and treatment. Multisectional assessment using both computerized tomography (CT) and magnetic resonance imaging (MRI) has always been a challenge due to the constant and complex movement of the heart.
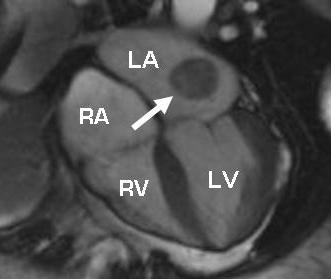
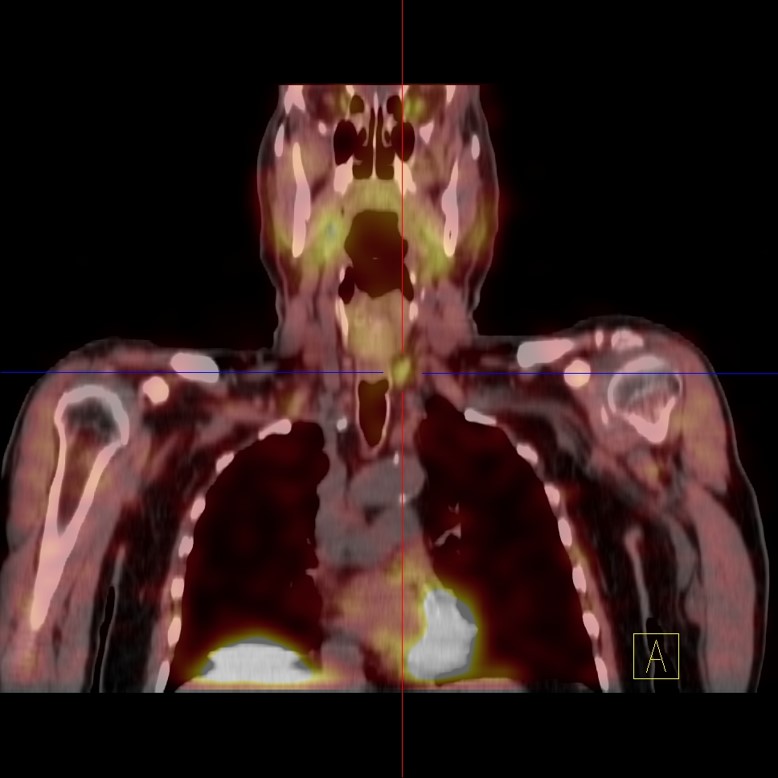
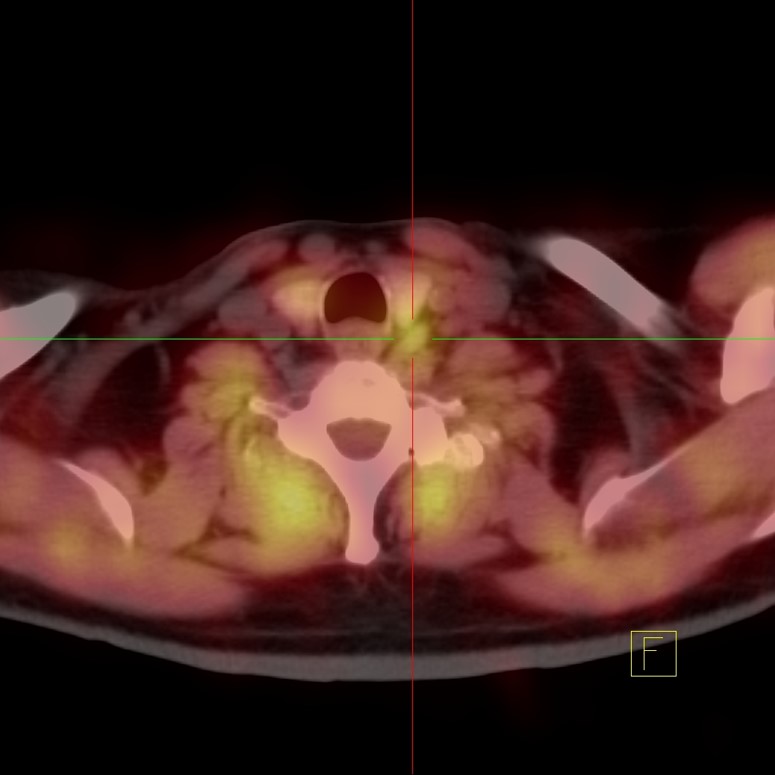
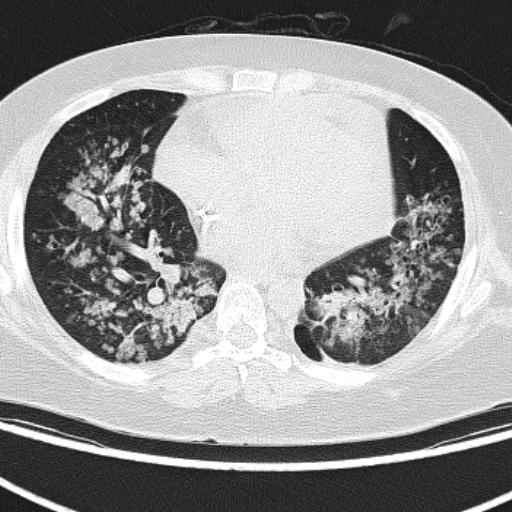
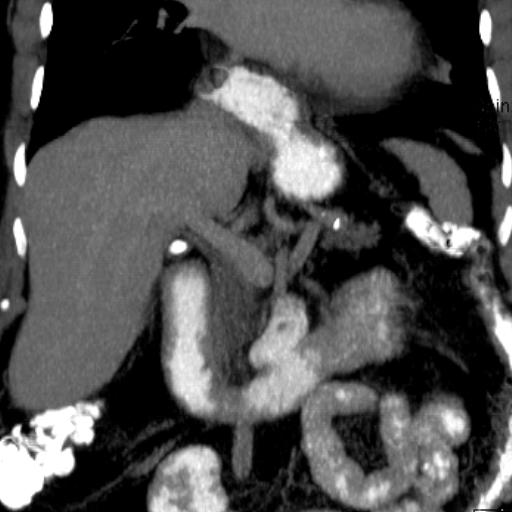
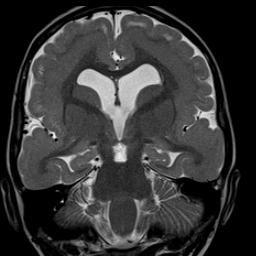
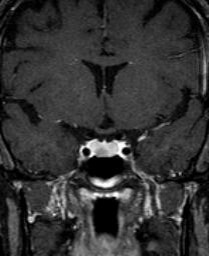
The first MRI images of the heart were obtained in 1982. Over the last 30 years the technique has evolved and today it has become an indispensable and complementary diagnostic and treatment tool in the most renowned specialized hospital and outpatient centers worldwide that are dedicated to treating cardiovascular conditions. MRI does not use radiation and does not require prior preparation, taking 45 minutes in most cases. It provides a multiplanar perspective of the heart’s anatomy (image 1) in all phases of the heart muscle (myocardium) contraction cycle by characterizing various patterns of pathology in the myocardium (cardiomyopathies) such as right ventricular arrhythmogenic dysplasia (image 2). MRI provides accurate and detailed information on the anatomy of the heart, the movement of the myocardium from the ventricles, the perfusion provided by arteries to the myocardium and its viability. Viability refers to determining whether the muscle is diseased but in time to be rescued by intervention (angioplasty or bridging with other arteries or veins from another part of the body) or whether it is dead or irreversibly scarred (no intervention would be beneficial). MRI obtains regular static images as in any other part of the body supplemented with images displayed in moving film format. Intravenous gadolinium contrast is essential for a complete MRI study of the heart. Certain types of heart attacks affect only the deeper layer called the subendocardium as opposed to the more extensive attacks that affect a more extensive thickness of the heart wall. MRI detects deep heart attacks better than any other imaging study, including nuclear medicine heart studies (Image 3). This modality also evaluates heart valves. Images 4 and 5 show the aortic valve while it is open and closed, respectively. Image 6 shows an incompetent aortic valve that does not close properly at the time it is supposed to close completely, allowing blood to return to the left ventricle. Figure 7 shows the mitral valve opening normally. The study also evaluates the thickness of the sac lining the heart (pericardium) by detecting the presence of abnormal fluid collections and masses. Image 8 shows a mass originating in the pericardium. Masses in other parts of the heart are also detectable and characterized by this modality, Image 9 showing the most common primary heart tumor, atrial myxoma.
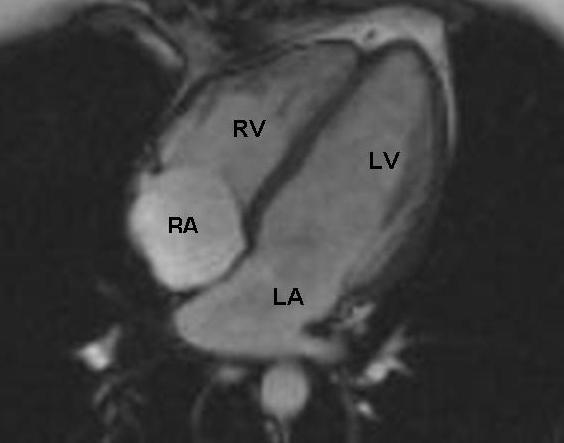
Image 1
Cardiac MRI, normal. 4 chamber view. RA right atrium_ RV right ventricle_ LA left atrium_ LV left ventricle
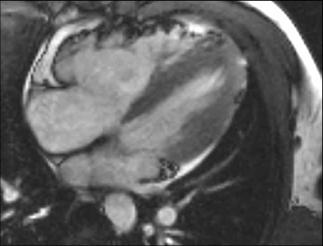
Image 2
Cardiac MRI, arrythmogenic right ventricular dysplasia (ARVD). Fatty replacement and microaneurysm of the right ventricle

Image 3
Cardiac MRI, arrows delineate a subendocardial infarct of the left ventricle, seen as a white band of enhancement

Image 4
Cardiac MRI, the bright triangle represents blood flowing across a normally open aortic valve, arrows delineating the valve perimeter
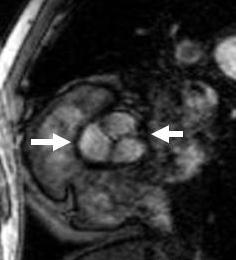
Image 5
Cardiac MRI, the three cusps of the aortic valve are fully closed
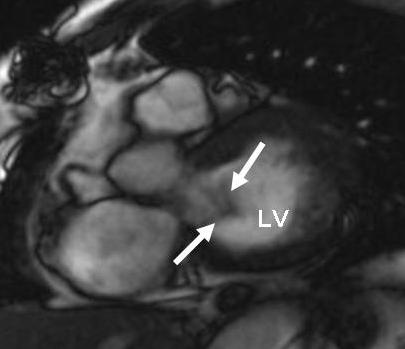
Image 6
Cardiac MRI, arrows point at blood that regurgitates or flows backward across an aortic valve that does not close properly
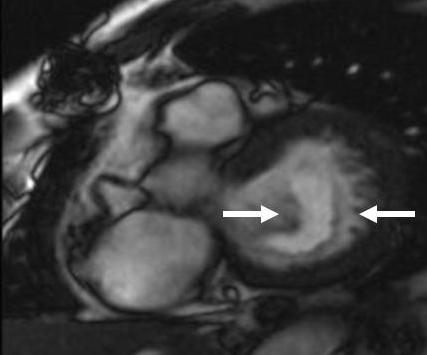
Image 7
Cardiac MRI, arrows point to the two open cusps of the mitral valve

Image 7
Cardiac MRI, mass in the left side of the heart arising from the pericardium, in this case a hemangioma