In this third brief, we will discuss clinical considerations relevant to intravenous contrast in Radiology (substances injected to achieve visualization of the vascular anatomic compartment, characterization of discernible lesions on non-contrast images and visualization of non-discernible lesions on non-contrast images). In particular we will focus on patients with drug allergies or iodine-based contrast; patients with renal insufficiency in reference to iodine-based contrast (CT/CTAngiography) and gadolinium-based contrast (MRI/MRAngiography); and diabetic patients taking oral hypoglycemic agents containing Metformin.
Patients with Drug Allergies or Allergies to Iodine-Based Contrast and History of Asthma Requiring Medication
It has been noted that those patients who have documented allergies to medications, to iodine-based contrast (used in CT and CTA, the next to disappear IVP and digital angiography/venography using catheterization), or with a history of asthma requiring medications are at a higher risk than the population without this history of developing an adverse reaction to both iodine-based and gadolinium-based intravenous contrast (used in MRI). As a protective measure, these patient categories are exposed to a reduced risk of adverse reaction if they receive a premedication that uses a combination of an antihistamine agent and steroids. Some have associated the routine addition of an H2 receptor blocking agent but this is not universally accepted. There are radiologic center uses the following: Medrol 20 mg po or Methylprednisolone 32 mg po at 12, 6, and 1 hour prior to iodine-based intravenous contrast administration and Diphenhydramine 25 mg po at 6 and 1 hour prior to contrast administration. Consult the staff in charge of your radiology center for details on your preferred regimen.
It is important to note that the patient should be aware that premediation medications will be administered prior to the intravenous injection of iodine or gadolinium-based contrast. Of course, it is imperative to establish that there is no history of allergy to the premediation components in which case the antihistamine agent is changed or the steroid is eliminated. Similarly, it is important to be clear about what the patient reports as an allergy. Often, the patient will indicate that food did not go down well or that he or she had a committee after a medication, clearly stating that this was not an allergy.
Often with a history of allergy to radiological contrast, when the patient indicates having experienced a “warmth” or a metabolic taste after receiving contrast, it should be made clear that this does not constitute an allergy but rather physiological sensations to be expected.
Some patients and physicians choose to prescribe premedication even when there are no risk factors mentioned above as a prophylactic measure. What is pertinent to explain to every patient is that premediation is not a guarantee that the patient will not experience an allergic reaction, including death; but a measure that has documented reduction in morbidity, but not necessarily in mortality.
Intravenous Iodine-Based Contrast and Renal Failure
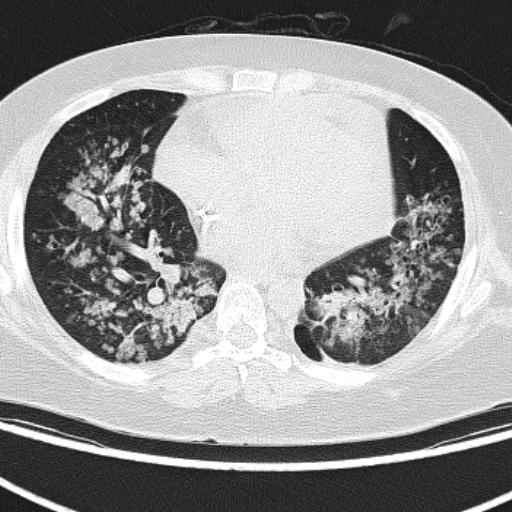
An increase in creatinine has been documented in patients immediately after receiving iodine-based contrast for CT scans and other radiological studies. In the vast majority of cases, renal function normalizes in the short term, but in a minority it does not normalize and eventually progresses to the development of nephropathy due to contrast. Both diabetic patients – particularly when dehydrated – and patients with paraproteinemia syndromes such as multiple myeloma and patients with collagen-vascular diseases are the patient groups most at risk for developing nephrotoxicity secondary to iodine-based contrast. Radiological centers and the referring physician should take steps to hydrate these patients well before, during and after iodine-based contrast injection to reduce the incidence of contrast-induced renal failure.
Patients with marginal renal disease are at a higher risk for developing renal failure due to iodine-based contrast than the rest of the population so alternatives such as performing the study without iodine-based contrast, performing the study with a reduced dose of iodine-based contrast or performing an MRI with gadolinium should be considered. Administration of the oral antioxidant N-acetylcysteine should be considered for patients at risk for developing iodine-based contrast-related nephropathy, but this measure should not replace hydration.
The consideration of iodine-based contrast-related nephropathy in patients on dialysis for end-stage renal disease (ESRD) does not apply due to the absence of renal function. Contrast is not protein bound and is of low molecular weight so it is easily dialyzed. The primary consideration in these patients when performing an iodine-based contrast radiologic study is the osmotic load they experience. Coordinate dialysis early after the radiologic study would apply in those patients who have compromised cardiac function or who will be receiving high volumes of iodine-based contrast media to avoid the likelihood of congestive heart failure.
Gadolinium-based Intravenous Contrast (MRI) and Renal Insufficiency
Because gadolinium is not considered nephrotoxic, it is recommended for patients who require a radiological tomographic study (CT or CTA) but have a contraindication to iodine-based contrast. Until recently gadolinium MRI contrast was not considered toxic for dialysis patients. Recently, cases of a new disease known as nephrogenic systemic fibrosis (NSF) have been reported in which a high correlation has been found between recent use and prolonged exposure to intravenous gadolinium in patients with significant renal insufficiency including ESRD. Also known as nephrogenic including ESRD. It is also known as nephrogenic Fibrosing Dermopathy. The condition progressively involves the skin and viscera resulting in death.
Because of this new information, preliminary (unpublished) recommendations by experts in intravenous contrast media for MRI and MRA suggest (verbal communication) for patients with significantly compromised renal function that both the referring physician and the radiologist make sure that there is a real indication for gadolinium. The dose of gadolinium should be reduced to the minimum possible. If the patient is dialyzed, dialysis should be scheduled the same day after the gadolinium MRI study. If the patient uses ambulatory peritoneal dialysis (9CAPD), an additional session should be scheduled for the day of the MRI study.
Diabetics Taking Oral Hypoglycemic Agents Containing Metformin at Risk for Developing Lactic Acidosis
Non-insulin-dependent diabetic patients who require iodine-based contrast typically for a CT scan (and other precisely listed modalities) and who take oral hypoglycemic agents containing Metformin are at risk for developing lactic acidosis which has proven to be fatal (50% mortality rate). Metformin is available both alone and in combination with other agents. The products metabolized when the liver receives the hypoglycemic agent, which are usually eliminated by the renal route, may remain in high concentration if iodine-based contrast would result in significant nephrotoxicity. The similar serious effect in patients with hepatic dysfunction may reduce the ability to metabolize lactic acid produced by Merformin. This is why it is indicated to suspend the hypoglycemic agent containing Metformin prior to the radiological study with iodine-based contrast injection, and for 48 hours after the study.
The physician in charge of the patient’s diabetes management should authorize this management in order to implement an alternate sugar control regimen. Often a specialist ordering a CT study with intravenous contrast by this physician is not in charge of the clinical-radiological management is imperative so that the patient is not put at risk unnecessarily. Once it is documented that renal function was not compromised, usually with a post CT scan serum creatinine, the hypoglycemic agent with Metformin is resumed.
At present, it is not necessary to discontinue Metformin when the diabetic patient undergoes an MRI study with routine doses of intravenous gadolinium. If the patient will receive high doses of gadolinium or has significantly compromised renal function, then discontinuation of Metformin should be considered.
The information presented is under continuous revision and should not be understood to represent the only or most recent recommendations available. An excellent source of information is the American College of Radiology Contrast Media Manual which is periodically updated. Maintaining close communication with your radiologist and nephrologist is imperative for optimal patient management when radiologic studies with intravenous contrast media are involved.
About the author:
Dr. Fernando Zalduondo Dubner, Director San Patricio MRI & CT Center, www.spmedflix.com, (787) 620-5757; (787) 766-1493.